Abstract
Post-concussion syndrome (PCS) refers to a constellation of physical, cognitive, and emotional symptoms after
traumatic brain injury (TBI). Despite its incidence and impact, the underlying mechanisms of PCS are unclear. We
hypothesized that impaired cerebral autoregulation (CA) is a contributor. In this article, we present our protocol
for non-invasively assessing CA in patients with TBI and PCS in a real-world clinical setting. A prospective, observational
study was integrated into outpatient clinics at a tertiary neurosurgical center. Data points included: demographics,
symptom profile (Post-Concussion Symptom Scale [PCSS]) and neuropsychological assessment
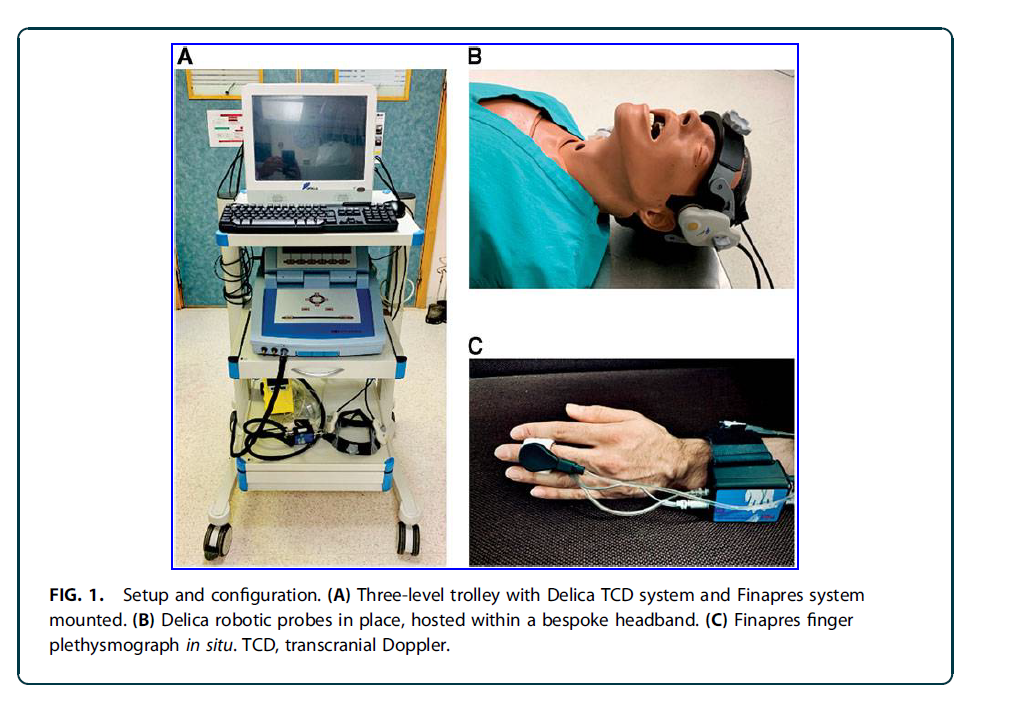
(Cambridge Neuropsychological Test Automated-Battery [CANTAB]). Cerebrovascular metrics (nMxa co-efficient
and the transient hyperaemic-response ratio [THRR]) were collected using transcranial Doppler (TCD), finger
plethysmography, and bespoke software (ICM ). Twelve participants were initially recruited but 2 were excluded
after unsuccessful insonation of the middle cerebral artery (MCA); 10 participants (5 patients with TBI, 5 healthy
controls) were included in the analysis (median age 26.5 years, male to female ratio: 7:3). Median PCSS scores
were 6/126 for the TBI patient sub-groups. Median CANTAB percentiles were 78 (healthy controls) and 25
(TBI). nMxa was calculated for 90% of included patients, whereas THRR was calculated for 50%. Median study
time was 127.5 min and feedback (n = 6) highlighted the perceived acceptability of the study. This pilot study
has demonstrated a reproducible assessment of PCS and CA metrics (non-invasively) in a real-world setting.
This protocol is feasible and is acceptable to participants. By scaling this methodology, we hope to test whether
CA changes are correlated with symptomatic PCS in patients post-TBI.